In 2021 and 2022, MinacNed will host pre-events leading up to the international MicroNanoConference 2022. The symposia are live events in The Netherlands, offering an interesting program with speakers from industry and science, with an opportunity for networking.
On November 23, a Micro Nano Symposium will be organised around the 2021 Groeifonds application. The consortium of partners from science and industry responsible for program will celebrate the submission of their application, specifically the focus theme Biomedical production technology under the NXTGen High Tech
From Science to Market: Biomedical Production Technology
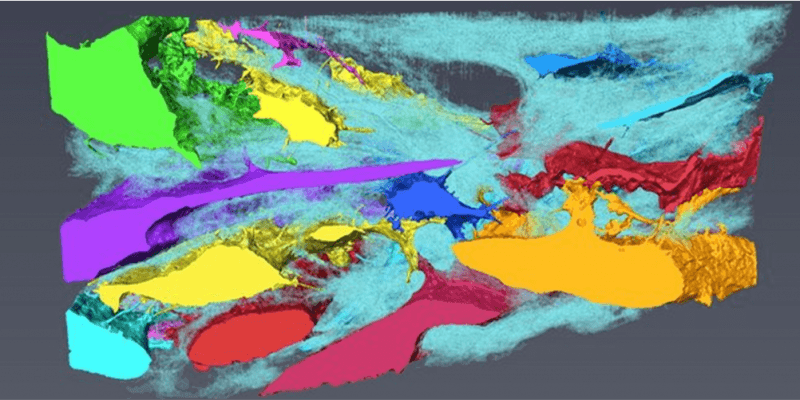
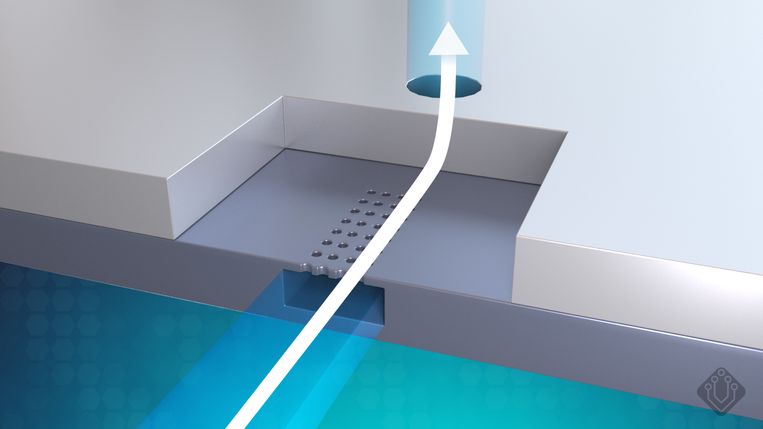
Biomedical production technology fails to keep pace with innovations in the biomedical domain. The (academic) knowledge in the Netherlands is at a very high level in the field of Lab-on-Chip, Organ-on-Chip, Artificial Organs and Cell production technology, but is not (properly) converted into products. The main reason for this is that a multidisciplinary chain is required of suppliers of high-quality specific components in both the technological and biological field. Although the required parties are present in the Netherlands, their production equipment and processes are not yet compatible with each other. These major challenges cannot be solved by a few parties, but a large collaboration is needed to be able to design and functionally qualify products from the existing developed building blocks (e.g., sensors, chips, biomaterials) in order to subsequently achieve upscaling and the growing (world) market.
MinacNed, hDMT, MESA+ and Nano4Society organize a pre-event of the international MicroNano Conference 2022 to address this topic and will present steps that are currently being taken to establish an ecosystem with a unique and first-of-its-kind production chain in the Netherlands.




Organizers: hDMT, MinacNed, MESA+, Nano4Society
Date: 23 November 2021, 14.00 – 17.00
Location: The Gallery, University of Twente, Enschede
(The Gallery, Hengelosestraat 500, 7521 AN Enschede)
Preliminary program
13.30 – 14.00 Arrival with coffee and tea
14.00 – 14.10 Opening and welcome, Janny van den Eijnden-van Raaij (chair, hDMT) and Albert van den Berg (MESA+)
14.10 – 14.40 Tom van der Horst (TNO), Overview NXTGEN HIGHTECH
14.40 – 15.10 Berend van Meer (hDMT): “A national ecosystem for biomedical production technologies”
15.10 – 15.40 Coffee Break and networking
15.40 – 16.10 Marko Blom (Micronit, Enschede), NXTGEN HIGHTECH: perspective from high tech industry: “Challenges and solutions for scaling from fabrication of prototypes to repetitive manufacturing”
16.10 – 16.40 Jasper Boomker (Kidney Foundation) NXTGEN HIGHTECH: perspective from end user: “Closing innovation gaps: the case of the artificial kidney”
16.40 – 17.00 Panel discussion
17:00-17:30 Drinks and networking
Invited keynote speakers include science and industry partners, a government overview of the importance of these partnerships and the point of view from an end user. After these great talks, the inspired attendees can meet and greet in a network setting with drinks to formalize future partnerships. The event is a live event in Enschede, at the location The Gallery.
You can now register (free of charge) to attend the event for one of the limited seats.
Registration Micro Nano Symposium
From Science to Market: Biomedical Production Technology